Robert Brown's patients may be obese or anorexic; sexual innocents or infected with chlamydia; male or female; jocks or goths; abusers of alcohol, Ecstasy, or over-the-counter drugs; tattooed, pierced, pimpled; surly and stressed; or just mortified by their molting, rebelling bodies.
Diverse and challenging, they share at least one common factor, which brings them to the attention of Brown and his colleagues. They are all adolescents.
"We do dermatology, sports medicine, psychology, gynecology, orthopedic issues, psychosocial issues, substance abuse, and address problems of developing sexuality," said Brown, a specialist in adolescent medicine who is chairman of pediatrics at Crozer-Chester Medical Center, in Upland, Pennsylvania.

PHOTO: NY TIMES NEWS SERVICE
"We're highly trained generalists for a specific population — like gerontologists," he said. "But either we've done a poor job of marketing ourselves or there is something about the field."
Adolescent medicine might be expected to be booming. The US has about 40 million people ages 10 to 19, a patient population that experts say is vulnerable to a growing array of behavior-related health problems.
But a decade after adolescent medicine became board certified in the US as a subspecialty, it is in little demand by doctors seeking to advance their careers. Small wonder the public is generally unaware of the field: according to the American Board of Medical Specialties, only 466 certificates in adolescent medicine were issued from 1996 to 2005. In the same period, 2,839 were issued in geriatric medicine.
Most major teaching hospitals have adolescent clinics: pediatric residents have to spend a month in an adolescent rotation. A few health maintenance organizations have stand-alone adolescent clinics. Occasionally, a pediatrician in a group practice or in a community may have a special affinity for teenagers, and be the go-to doctor for them.
But the availability of doctors and nurse practitioners dedicated exclusively to adolescent care is still the exception. Their numbers are so limited that many cannot take on adolescents as primary-care patients; the patients see them on a temporary referral basis. Of those teenagers who are insured and who continue to see a primary-care doctor, a vast majority remain with the pediatricians or family doctors who have cared for them since diaperhood.
That job has become more time-consuming and complex. "Adolescents are not big children and they're also not little adults," said Walter D. Rosenfeld, an adolescent medicine specialist and chairman of pediatrics at the Goryeb Children's Hospital, in Morristown, New Jersey.
They are not just a bridge population, he and many others maintain, but their own stop in the road. During adolescence, people need to learn how to take responsibility for their health and, eventually, to become health care consumers, independent of their parents.
At programs that are sensitive to adolescents, this changing dynamic is negotiated deftly but firmly. Recently, at an eating disorder clinic at the Goryeb Children's Center, at Overlook Hospital in Summit, New Jersey, a nutritionist beckoned to a teenager in the waiting area. The girl's mother stood to follow. But after the girl slipped into the exam room, the nutritionist closed the door.
"Oh, I thought I was going in with her," the mother said to no one in particular. "Guess not," she added with a small laugh of embarrassment.
Organizations like the American Academy of Pediatrics and the Society for Adolescent Medicine recommend that primary-care physicians monitor teenagers for drug and alcohol use, smoking, sexual activity (including disease prevention and use of birth control), physical activity, nutrition, depression, school behavior, and social pressures. Yet various studies have shown that many pediatricians feel inadequately prepared to address most of these issues.
A father in Indianapolis, who did not want to identify himself to protect the privacy of his shy 12-year-old daughter, said: "Our pediatrician is a great guy around everyday things, but he's not adolescent-focused. He won't ask her about sex or alcohol or drugs. It's just not in his repertoire. He's a baby doctor, oriented toward the quickie office visit."
Because teenagers seek out doctors infrequently, pediatricians have to grab at any opportunity to reach them, said Susan Brill, director of adolescent medicine at the Children's Hospital at St. Peter's University Hospital, in New Brunswick, New Jersey.
"I could see a boy with strep throat and he'll grunt at me and we'll be done in five minutes," she said. "Or I could take a little more time to talk to him — I might find out about sexuality issues that way. If a kid is coming in for bronchitis, I'll get the parent out of the room and ask the kid if he's smoking. If a kid is on a sports team and comes in with an injury, is the pediatrician talking about weight and eating and steroid abuse?"
With so many doctors feeling underprepared to treat teenagers and the need so critical, why no rush to those advanced degrees?
In conventional terms, the explanations for adolescent medicine's remaining the wallflower at the subspecialty ball are sensible enough. The fellowship is demanding: two years of additional study for internists and family practitioners, three for pediatricians.
Yet after completing the adolescent fellowship, a doctor's income does not markedly improve. Insurance companies still view teenagers as large children. Though the annual checkup of a 16-year-old should take at least twice as long as that of a 6-year-old, doctors say, the typical reimbursement is about the same.
Moreover, the field does not get much respect, at least from other doctors (parents can be weepy with gratitude). In the thriving world of high-tech medicine, doctors who treat adolescents are determinedly low-tech. They listen. They observe. They do some subtle teaching, a fair amount of diagnosing and, on the good days, intervention, amelioration, even outright prevention.
And then there are the patients themselves.
"American society is not particularly fond of its teenagers," said John Santelli, a professor of pediatrics and public health at Columbia University. "The 2-year-olds, everyone fawns over them. But the guy with the pin through his nose is not cute."
A 1999 American Academy of Pediatrics study revealed that while 22 percent of the patients seen by pediatricians were ages 12 to 18, 75 percent of the doctors surveyed did not want more adolescents in their practice.
The meager reimbursement rates directly affect pediatricians and family doctors. Elizabeth Panzner, a pediatrician in Union, New Jersey, who speaks joyfully about watching a patient grow over many years, said adolescents were nonetheless a challenge for a busy practice.
"Say there's a gynecological issue," she said. "Putting the time factor aside, there's a financial burden which the pediatrician would never recoup because gynecological visits are bundled into a general pediatric office visit."
A relatively tiny, hardy, occasionally eccentric and fervent group, adolescent-medicine specialists understand that theirs will probably never become a much-sought-after position. Many have come to see their mission not only in taking care of patients, but also in researching public policy questions that affect adolescents.
And because many choose to become affiliated with hospital programs rather than setting up fee-for-service practices, they also teach pediatric residents and local practitioners how to exchange critical information with teenage patients.
"We can't do it alone," Rosenfeld, the specialist in Morristown, said. "We need to deputize pediatricians and family practitioners, and make them our partners."
Since October, specialists in adolescent medicine in his department have given a half-dozen lectures, including one for the professionals at a local pediatric practice, as well as those for pediatric residents on dating violence and eating disorders.
They have also tried direct outreach to adolescents: last year, their blunt Web site, www.teenhealthfx.com, which has an advisory board of teenagers, averaged nearly a quarter-million hits a month.
Kenneth R. Ginsburg, an adolescent-medicine specialist at Children's Hospital of Philadelphia who trains doctors in treating teenagers, said that when the child is 11 to 13, the doctor should explain to both patient and parent that the visit will change: the doctor will now spend some of it alone with the patient.
Parents need to be assured, Ginsburg said, that although they will now be left in the dark about some of what is said in the exam room, the doctor's goal is still the health and well-being of their child.
The challenge, then, he and other experts say, is how to speak with teenage patients using language that is nonjudgmental and does not make them feel ashamed.
Leslie Sanders, an adolescent medicine specialist at Overlook, recently gave a lecture to pediatric residents about interviewing teenage boys. "Many pediatricians know they should be asking, but don't know how," she said. "They might say, 'You know how to put on a condom, don't you?' or 'After you drink, you don't get behind the wheel, right?'"
When Ginsburg sits down with teenagers, he lays out the deal: "They'll have a choice: they can say they don't want to talk about this subject. They can lie to me, but if they do, I can't help them. Then I emphasize the importance of honesty.
"When the young person tells me something I wish they weren't doing, like drugs," Ginsburg said, "I won't praise the behavior but I'll respect the fact that they're talking to me and looking for guidance. The kid needs to know that my office is a place where they can get out of trouble, but not in trouble."
Doctors who choose to treat teenagers exclusively have a special affection for them. Ginsburg's patients include the children of intellectuals and the privileged as well as those living in shelters and foster homes. For many of these doctors, the work has both a tinge of personal identification and a call to social conscience. Santelli, who is also a family planning expert, remarked: "We all have our adolescence to live down. It was an important time to me, personally. So I resonate when I talk to teenagers."
"Adolescence is at the intersection of fundamental issues for society: if you make it through successfully, you're set up for life," Santelli said. "If you don't, you could go to prison or end up in the underclass."
These doctors are also clear-eyed about their patients. This is, after all, a patient population whose three leading causes of death — accidents, homicide and suicide — are often related to psychosocial problems, rather than traditional medical diagnoses.
That is why a doctor-patient relationship with the teenager based on trust and confidentiality is so crucial, Ginsburg said.
"Adolescents are incredibly thoughtful, creative, and absolutely challenging," he said. "They get when you're insincere really quickly. The tough kids are not used to adults not fearing them. But if you just love being with them, they melt. The attitude goes away because it's just a pained, defensive posture."

In late October of 1873 the government of Japan decided against sending a military expedition to Korea to force that nation to open trade relations. Across the government supporters of the expedition resigned immediately. The spectacle of revolt by disaffected samurai began to loom over Japanese politics. In January of 1874 disaffected samurai attacked a senior minister in Tokyo. A month later, a group of pro-Korea expedition and anti-foreign elements from Saga prefecture in Kyushu revolted, driven in part by high food prices stemming from poor harvests. Their leader, according to Edward Drea’s classic Japan’s Imperial Army, was a samurai

The following three paragraphs are just some of what the local Chinese-language press is reporting on breathlessly and following every twist and turn with the eagerness of a soap opera fan. For many English-language readers, it probably comes across as incomprehensibly opaque, so bear with me briefly dear reader: To the surprise of many, former pop singer and Democratic Progressive Party (DPP) ex-lawmaker Yu Tien (余天) of the Taiwan Normal Country Promotion Association (TNCPA) at the last minute dropped out of the running for committee chair of the DPP’s New Taipei City chapter, paving the way for DPP legislator Su
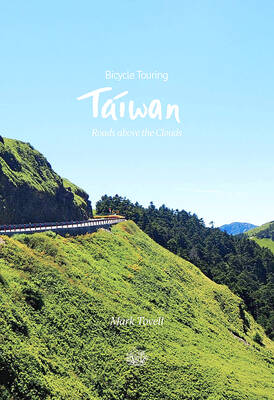
It’s hard to know where to begin with Mark Tovell’s Taiwan: Roads Above the Clouds. Having published a travelogue myself, as well as having contributed to several guidebooks, at first glance Tovell’s book appears to inhabit a middle ground — the kind of hard-to-sell nowheresville publishers detest. Leaf through the pages and you’ll find them suffuse with the purple prose best associated with travel literature: “When the sun is low on a warm, clear morning, and with the heat already rising, we stand at the riverside bike path leading south from Sanxia’s old cobble streets.” Hardly the stuff of your

Located down a sideroad in old Wanhua District (萬華區), Waley Art (水谷藝術) has an established reputation for curating some of the more provocative indie art exhibitions in Taipei. And this month is no exception. Beyond the innocuous facade of a shophouse, the full three stories of the gallery space (including the basement) have been taken over by photographs, installation videos and abstract images courtesy of two creatives who hail from the opposite ends of the earth, Taiwan’s Hsu Yi-ting (許懿婷) and Germany’s Benjamin Janzen. “In 2019, I had an art residency in Europe,” Hsu says. “I met Benjamin in the lobby