At 5 o'clock one morning in late March, Linda Dixon stood in the stream of an open fire hydrant as emergency medical workers flushed her chest, arms and face with water.
Dixon, a 42-year-old home health aide in Queens, New York, said her estranged boyfriend, the father of her three children, had gone into her bedroom and thrown acid on her after a confrontation.
Dixon was taken to the NewYork-Presbyterian/Weill Cornell hospital, where she underwent two surgeries for the worst of her injuries, a third-degree burn across her chest. The surgical team's first priorities were to remove as much of the burned skin as possible (it can easily become infected) and to cover the wound temporarily with skin from a cadaver.

Cadaver skin is removed from donors shortly after their deaths, then processed and distributed by skin and tissue banks. It has long been the preferred option for a patient with the most severe burns until a graft of the patient's own skin can be applied. Although some synthetic skin has come on the market in the last 20 years, new products have not appeared as quickly as some experts expected.
And experts now realize that cadaver skin is unlikely to be replaced as a treatment option anytime soon.
"Cadaver skin still is probably the No. 1 substitute for the patient's own skin" in acute cases, said Roger Yurt, professor of surgery and director of the Hearst Burn Center. Yurt also oversees the hospital's dedicated skin bank, called the New York Firefighters Skin Bank.

Palmer Bessey, professor of surgery and associate director of the burn center, said cadaver skin was particularly valuable in cases like Dixon's, when the burn may penetrate deeper than is immediately apparent. Initially, it may not be clear whether the bed of the wound will be able to accept a graft, and under such circumstances, synthetics are more prone to infection than cadaver skin, Bessey said.
In Dixon's case, Bessey decided to use strips of cadaver skin, which had been frozen at the hospital's skin bank. In the operating room, these strips were thawed in a small tub of saline.
They were rolled through a meshing machine, which created a pattern of small holes, like the pattern in fishnet stockings. This allowed the cadaver skin to be stretched to cover a broader area of Dixon's chest. It also allowed for better drainage of the wound because blood clots or fluid could seep through the perforations and not get stuck under the graft.
Donated skin can help prevent infection, reduce pain and maintain body temperature. Patients with severe burns do not initially reject cadaver skin, because their immune systems are suppressed, Bessey said.
Each strip is about 0.33mm thick, roughly the thickness of sunburned skin. The strip includes the dull outer layer, or epidermis, and a small portion of the shiny inner layer, or dermis. Both are destroyed in a third-degree or full-thickness burn.
When a skin bank receives a call about a potential donor, an extensive screening process begins -- for risk factors associated with HIV, hepatitis, cancer, mad cow disease and even Chagas' disease, a parasitic infection.
"A large proportion of potential donors are rejected," said Nancy Gallo, the administrative director of the Firefighters Skin Bank and a registered nurse.
When donors are accepted and their families consent, a team from the skin bank goes to the hospital and surgically removes roughly 122 square centimeters of a cadaver's skin. The skin is taken to the skin bank, trimmed into bandage-like strips and cryogenically preserved. Cadaver skin can be stored in a freezer for up to five years, although it is invariably needed sooner.
"We are always in need of more skin," Gallo said, adding that the skin bank faces a declining number of donors. "Right now there is a national shortage."
She added that she frequently received calls from people planning to undergo gastric bypass surgery, a surgical treatment for obesity, who would like to donate skin. But given current skin harvesting procedures, this is not an option.
According to Bessey, Dixon responded well to the graft of donated skin, which integrated into her body and helped the area begin healing. Bessey then performed a second operation, removing the cadaver material and replacing it with Dixon's own skin, taken from her thigh.
"I was very scared," Dixon said. But she added that she was in less pain then than she was before the operations.
Most of the less severe burns on Dixon's face are healing naturally. The burn on her right eyelid was too deep to heal by itself, and a graft of her own skin was applied during the second operation, Bessey said.
Richard Kagan, professor of surgery at the University of Cincinnati College of Medicine and chief of staff at the Shriners Burns Hospital in Cincinnati, said that for temporary wound coverage for acute burns, cadaver skin has been the best option for more than 40 years.
"The development of a permanent, off-the-shelf skin replacement has been much slower than had been anticipated," he said, although, he added, "some of the synthetics do have advantages."
Integra artificial skin products, from Integra LifeSciences, are among the most widely used synthetics. Its first skin product received approval from the Food and Drug Administration in 1996 and consisted of two layers: an inner scaffold on which the dermis could redevelop and an outer layer of silicone.
Other skin products, approved in 2002, made small improvements but were not substantially different, according to a company spokeswoman.
Integra's artificial skin products have advantages over cadaver skin in that they are easier to store. Because they help to rebuild the inner, structural layer of skin, they can improve the appearance of a scar. They can also reduce the amount of scarring that contracts around a joint or other areas that requires mobility.
But these products cost more than cadaver skin, Kagan and others say. The products can also be hard to handle and may be more prone to infection, particularly when placed on a wound of questionable viability. And, like patients given cadaver skin, those given artificial skin products must eventually receive grafts of their own skin.
A product called Epicel, introduced by Genzyme Biosurgery in the 1980s, offers a permanent replacement for a patient's outer skin. It consists of a sheet of epidermis, grown and cultured over several weeks from a sample of a patient's own skin cells.
Along similar lines, Steven Boyce, professor of surgery at the University of Cincinnati and a senior researcher at the Shriners Burns Hospital, has developed a laboratory process in which both epidermis and some dermis can be produced in about a month using cells isolated from a patient's skin and grown in culture.
This product, PermaDerm, is being developed by the Cambrex Corp. It is not available now on a large scale. But even it is not a skin replacement that can be used immediately for any permanent wound closure. And for many researchers, such a product remains the dream.

In late October of 1873 the government of Japan decided against sending a military expedition to Korea to force that nation to open trade relations. Across the government supporters of the expedition resigned immediately. The spectacle of revolt by disaffected samurai began to loom over Japanese politics. In January of 1874 disaffected samurai attacked a senior minister in Tokyo. A month later, a group of pro-Korea expedition and anti-foreign elements from Saga prefecture in Kyushu revolted, driven in part by high food prices stemming from poor harvests. Their leader, according to Edward Drea’s classic Japan’s Imperial Army, was a samurai

The following three paragraphs are just some of what the local Chinese-language press is reporting on breathlessly and following every twist and turn with the eagerness of a soap opera fan. For many English-language readers, it probably comes across as incomprehensibly opaque, so bear with me briefly dear reader: To the surprise of many, former pop singer and Democratic Progressive Party (DPP) ex-lawmaker Yu Tien (余天) of the Taiwan Normal Country Promotion Association (TNCPA) at the last minute dropped out of the running for committee chair of the DPP’s New Taipei City chapter, paving the way for DPP legislator Su
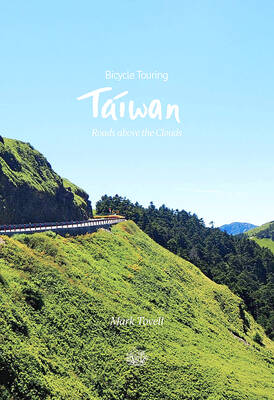
It’s hard to know where to begin with Mark Tovell’s Taiwan: Roads Above the Clouds. Having published a travelogue myself, as well as having contributed to several guidebooks, at first glance Tovell’s book appears to inhabit a middle ground — the kind of hard-to-sell nowheresville publishers detest. Leaf through the pages and you’ll find them suffuse with the purple prose best associated with travel literature: “When the sun is low on a warm, clear morning, and with the heat already rising, we stand at the riverside bike path leading south from Sanxia’s old cobble streets.” Hardly the stuff of your

Located down a sideroad in old Wanhua District (萬華區), Waley Art (水谷藝術) has an established reputation for curating some of the more provocative indie art exhibitions in Taipei. And this month is no exception. Beyond the innocuous facade of a shophouse, the full three stories of the gallery space (including the basement) have been taken over by photographs, installation videos and abstract images courtesy of two creatives who hail from the opposite ends of the earth, Taiwan’s Hsu Yi-ting (許懿婷) and Germany’s Benjamin Janzen. “In 2019, I had an art residency in Europe,” Hsu says. “I met Benjamin in the lobby