There was little that doctors could do for a 3-year-old boy brought to Bangkok’s main children’s hospital two weeks ago with dengue fever. Like thousands before him, he had reached the most dangerous phase of the disease, dengue shock syndrome, and he died of internal bleeding and organ failure three days after being admitted.
Directly across the street, in the US Army’s largest overseas medical research laboratory, military scientists are offering hope for future generations: a vaccine. Developed after decades of trying, it is one of two experimental vaccines that experts believe may be commercially available in about 6 years.
Dengue, a mosquito-borne illness once known as breakbone fever for its intense joint and muscle pain and crushing headaches, has a relatively low death rate — about 2.5 percent of hospitalized patients, the WHO reports. But because patients can require constant, careful monitoring, it is one of the costliest diseases in tropical countries. Each year, it leads to about 500,000 hospitalizations around the world.
Dengue is seldom seen in the US or Europe, though it is the second-most common cause (after malaria) of feverish symptoms for Western tourists returning from developing countries.
But it is important to the Army: American soldiers have contracted dengue as recently as the 1990s, on missions in Haiti and Somalia. So it is one of the tropical diseases that are the focus of research here at the Armed Forces Research Institute of Medical Sciences, which the Army has operated with the Royal Thai Army for five decades.
The research center, which employs several hundred people, is housed in an unremarkable 1960s building alongside a greasy alley where food vendors hawk fried grasshoppers and freshly mashed papaya salad.
“There’s no dengue in Kansas,” said Colonel James Boles, the commander at the laboratory. “No malaria, either. That’s why we are here.”
A FORMIDABLE FOE OFF THE BATTLEFIELD
In wars past, disease has often proved a greater foe than opposing armies. During the Anglo-Boer War in South Africa in the late 19th century, more soldiers died of typhoid than in battle. Thousands of cases of hepatitis during the Vietnam War among soldiers spurred Army researchers to help develop two of the vaccines now in use to prevent hepatitis A and B.
“All we care about is that we get a vaccine that protects soldiers,” said Lieutenant Colonel Stephen Thomas, a medical doctor who is director of dengue vaccine development in the Bangkok laboratory. “Fortunately, a lot of our concerns are also global health concerns.”
For many years, the leading drugs used to treat malaria were developed by the Army. Today, research on tropical diseases is spread across a broader constellation; in the hunt for a dengue vaccine, money and research have come from the Thai government, nonprofit organizations like the Bill and Melinda Gates Foundation, and drug companies like GlaxoSmithKline, which is working with the Army.
The other vaccine at an advanced stage of development is being jointly developed by the French drug company Sanofi-Aventis and a Thai university on the same Bangkok street as the Army lab.
“We’re further along with the dengue vaccine than we’ve ever been,” said Duane Gubler, director of the emerging infectious diseases department of the Duke-NUS Graduate Medical School in Singapore. “There’s a good possibility that we’ll have a vaccine in five to seven years.”
The dengue virus is transmitted mainly by a mosquito called Aedes aegypti, which survives on human blood. Aedes rarely travels more than about 90m from its birthplace and thrives in populated areas.
The WHO estimates that 50 million people are infected every year. But most of those infected, perhaps as many as 90 percent, experience only minor flulike symptoms or none at all.
In more serious cases, like that of the boy who died here last month, symptoms include severe headaches, rapid onset of a high fever, debilitating joint and muscle pain, nausea, vomiting and internal bleeding. Generally, though, dengue is considered treatable as long as patients are brought to the hospital on time and the disease is properly diagnosed.
Scientists believe the disease has existed for centuries — an outbreak appears to have occurred in Philadelphia in 1780 — but dengue has become more common and more virulent over the past half-century.
In 1970, only nine countries were known to have had epidemics of the most serious form of the disease, dengue hemorrhagic fever. By the mid-1990s that number had quadrupled, and experts say the disease is particularly well adapted to an age of air travel and international trade.
There are four types of dengue virus. Patients who have been infected with one of them are believed to develop immunity to that type only — and, paradoxically, are more vulnerable to dengue hemorrhagic fever if they are exposed to a second type.
The four types have intermixed as people carried them on airplanes to far-flung places; outbreaks of the hemorrhagic fever have been traced to specific flight paths and trade routes.
“What we’ve done is provided the ideal mechanism for these viruses to move around the world,” said Gubler, who has researched dengue for nearly four decades.
STARTED WITH SOLDIERS
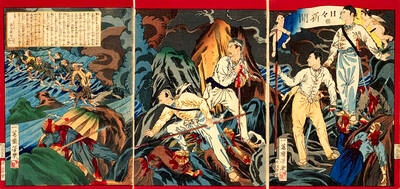
It was probably soldiers who caused the original spread of dengue hemorrhagic fever around Southeast Asia, during World War II.
“You had a movement of soldiers from England, the US, Australia and Japan,” said Suchitra Nimmannitya, a pioneer in dengue research who developed a handbook on how to treat the disease.
A Japanese scientist first isolated the virus during the war, and a US Army physician, Albert Sabin, made the discovery that there were distinct virus types. (Sabin went on to help develop the polio vaccine.)
The development of a vaccine is especially difficult because it will need to counter all four types of virus.
“If dengue was a single virus we would have had a vaccine already, for sure,” said Jean Lang, director of research and development at Sanofi’s emerging vaccine program.
Sanofi’s dengue vaccine, which will undergo trials in 4,000 children in Thailand in a few months, is one of the first vaccines to be produced using genetic engineering.
The Army’s vaccine, which is at a similar stage of development and has been tested on volunteers in the US, Puerto Rico and Thailand, was produced using live, attenuated viruses, a more traditional technique. The two or three doses, spaced months apart, are administered by injection.
Experts say the wide array of researchers involved — some with profit motives and others without — increases the chances of success and could help make the vaccine affordable to people in developing countries.

In the March 9 edition of the Taipei Times a piece by Ninon Godefroy ran with the headine “The quiet, gentle rhythm of Taiwan.” It started with the line “Taiwan is a small, humble place. There is no Eiffel Tower, no pyramids — no singular attraction that draws the world’s attention.” I laughed out loud at that. This was out of no disrespect for the author or the piece, which made some interesting analogies and good points about how both Din Tai Fung’s and Taiwan Semiconductor Manufacturing Co’s (TSMC, 台積電) meticulous attention to detail and quality are not quite up to

April 21 to April 27 Hsieh Er’s (謝娥) political fortunes were rising fast after she got out of jail and joined the Chinese Nationalist Party (KMT) in December 1945. Not only did she hold key positions in various committees, she was elected the only woman on the Taipei City Council and headed to Nanjing in 1946 as the sole Taiwanese female representative to the National Constituent Assembly. With the support of first lady Soong May-ling (宋美齡), she started the Taipei Women’s Association and Taiwan Provincial Women’s Association, where she
It is one of the more remarkable facts of Taiwan history that it was never occupied or claimed by any of the numerous kingdoms of southern China — Han or otherwise — that lay just across the water from it. None of their brilliant ministers ever discovered that Taiwan was a “core interest” of the state whose annexation was “inevitable.” As Paul Kua notes in an excellent monograph laying out how the Portuguese gave Taiwan the name “Formosa,” the first Europeans to express an interest in occupying Taiwan were the Spanish. Tonio Andrade in his seminal work, How Taiwan Became Chinese,

Mongolian influencer Anudari Daarya looks effortlessly glamorous and carefree in her social media posts — but the classically trained pianist’s road to acceptance as a transgender artist has been anything but easy. She is one of a growing number of Mongolian LGBTQ youth challenging stereotypes and fighting for acceptance through media representation in the socially conservative country. LGBTQ Mongolians often hide their identities from their employers and colleagues for fear of discrimination, with a survey by the non-profit LGBT Centre Mongolia showing that only 20 percent of people felt comfortable coming out at work. Daarya, 25, said she has faced discrimination since she