The heat source is a pair of headlights. A car door alarm signals emergencies. An auto air filter and fan provide climate control.
But this contraption has nothing to do with transportation. It is a sturdy, low-cost incubator, designed to keep vulnerable newborns warm during the first fragile days of life.
Unlike the notoriously high-maintenance incubators found in neonatal intensive care units in the US, it is easily repaired, because all of its operational parts come from cars.
And while incubators can cost US$40,000 or more, this one can be built for less than US$1,000.
The creators of the car parts incubator — a project being promoted by the Global Health Initiative at the Center for Integration of Medicine and Innovative Technology, or CIMIT, a nonprofit consortium of Boston teaching hospitals and engineering schools — say it could prevent millions of newborn deaths in the developing world.
The main causes of newborn death — infections, preterm birth and asphyxiation — are readily treatable with the right expertise and equipment, said Kristian Olson, principal investigator on the project. He called them the “low-hanging fruit” of global health interventions.
“It’s so frustrating to see these preventable deaths,” he said. “They won’t name babies in Aceh, Indonesia, until they’re two months old. It’s a cultural adaptation to expect a death.”
Mechanically, incubators are simple devices, providing a warm, clean, womblike environment in which a baby can mature (though state-of-the-art models may have accessories like built-in X-ray machines and rotating mattresses). Low birth weight and other problems make it especially difficult for newborns to regulate their body temperature, a condition that can lead to organ failure.
REPLACEMENT PARTS ... VIRTUALLY LIMITLESS
In the car parts incubator, infants born at 32 weeks’ gestation or longer can receive supplemental oxygen while their lungs gain strength, antibiotics if they have infections, and low-lit quiet in which to sleep if their mothers are away or are otherwise unable to hold them. In an emergency, the incubator’s bassinet can be removed and carried to another part of the building or even to another hospital.
In truth, experts say, the developing world doesn’t need more incubators. It needs incubators that work. Over the years, thousands have been donated from rich nations, only to end up in “incubator graveyards” — most broken, some never opened. According to a study from Duke University last year, 96 percent of foreign-donated medical equipment fails within five years of donation — mostly because of electrical problems, like voltage surges or brownouts or broken knobs, or because of training problems, like neglecting to send user manuals along with the devices.
To compensate for this philanthropic shortsightedness, medical staffs either crank up the temperature in “incubator rooms” to 37.8ºC or more, or swaddle babies in plastic to hold in body heat.
Such makeshift solutions led the Boston team to ask: How can we make an incubator for the developing world that will get fixed?
One person pondering that question in 2006 was Jonathan Rosen, then director of CIMIT’s technology implementation program. A proponent of sustainable biomedical technology, Rosen, now at the Boston University School of Management, uses the term “organic resourcing” to describe the principle of fashioning medical devices from whatever materials were locally abundant.
In his discussions with doctors who practice in impoverished settings, Rosen learned that no matter how remote the locale, there always seemed to be a Toyota 4Runner in working order.
It was his “Aha!” moment, he recalled later: Why not make the incubator out of new or used car parts, and teach local auto mechanics to be medical technologists?
CIMIT then hired Design That Matters, a nonprofit firm in Cambridge, Massachusetts, to design the machine. “The idea was to start with a 4Runner,” said Timothy Prestero, the firm’s founder
and chief executive, “and take away all the parts that weren’t
an incubator.”
What resulted was a serious-looking gray-blue device that conjures up a cyborg baby buggy, but fits comfortably in hospitals and clinics with few resources. For one thing, the supply of replacement parts is virtually limitless, because the modular prototype can be adapted to any make or model
of car.
“Junkyards are great sources for parts,” said Robert Malkin, director of Engineering World Health, a program based at Duke University, who is not affiliated with the incubator project. “We have designs for pumps and a surgical aspirator that are based on car parts.”
And the repair people will be right on the scene. “The future medical technologists in the developing world,” Malkin said, “are the current car mechanics, HVAC repairmen, bicycle shop repairmen. There is no other good source of technology-savvy individuals to take up the future of medical device repair and maintenance.”
Not everyone agrees that the car parts incubator is the best
solution for infant deaths. Skeptics cite a 2005 series of articles in the British journal The Lancet listing proven interventions — including outreach visits during pregnancy, skilled care at delivery and emergency treatment afterward — that could eliminate up to 72 percent of neonatal deaths worldwide.
THE POTENTIAL TO SAVE LIVES
The car parts incubator has received US$150,000 in initial financing from CIMIT. The project team is looking for foundation support to develop a working prototype.
Meanwhile, the team is refining its business model and solidifying business partnerships abroad. “The technology is the least difficult part of the problem,” Prestero said. “Manufacturing, financing, distribution, regulatory approval: those are major barriers. There aren’t many examples of a successfully scaled product to serve the poor.”
Olson says his determination to create a cheap, reliable incubator — and medical training to go with it — was reinforced on a trip this year to Cut Nyak Dhien Hospital, a one-story concrete building in the tsunami-stricken city of Meulaboh, Indonesia.
“When I walked in the incubator room,” he said, “a whole family was sobbing around a crib.” Their seven-day-old baby boy, who was born slightly underweight and suffering from infection, had just died, after lying for hours on a cold cot. With warmth and proper care, he would have survived.
Crowding the room were six donated high-tech incubators from the West. None of them worked.

In late October of 1873 the government of Japan decided against sending a military expedition to Korea to force that nation to open trade relations. Across the government supporters of the expedition resigned immediately. The spectacle of revolt by disaffected samurai began to loom over Japanese politics. In January of 1874 disaffected samurai attacked a senior minister in Tokyo. A month later, a group of pro-Korea expedition and anti-foreign elements from Saga prefecture in Kyushu revolted, driven in part by high food prices stemming from poor harvests. Their leader, according to Edward Drea’s classic Japan’s Imperial Army, was a samurai

The following three paragraphs are just some of what the local Chinese-language press is reporting on breathlessly and following every twist and turn with the eagerness of a soap opera fan. For many English-language readers, it probably comes across as incomprehensibly opaque, so bear with me briefly dear reader: To the surprise of many, former pop singer and Democratic Progressive Party (DPP) ex-lawmaker Yu Tien (余天) of the Taiwan Normal Country Promotion Association (TNCPA) at the last minute dropped out of the running for committee chair of the DPP’s New Taipei City chapter, paving the way for DPP legislator Su
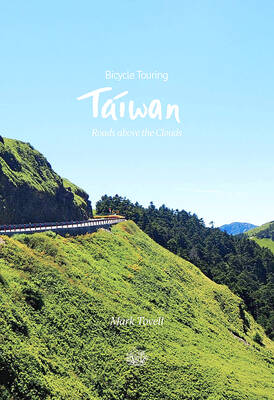
It’s hard to know where to begin with Mark Tovell’s Taiwan: Roads Above the Clouds. Having published a travelogue myself, as well as having contributed to several guidebooks, at first glance Tovell’s book appears to inhabit a middle ground — the kind of hard-to-sell nowheresville publishers detest. Leaf through the pages and you’ll find them suffuse with the purple prose best associated with travel literature: “When the sun is low on a warm, clear morning, and with the heat already rising, we stand at the riverside bike path leading south from Sanxia’s old cobble streets.” Hardly the stuff of your

April 22 to April 28 The true identity of the mastermind behind the Demon Gang (魔鬼黨) was undoubtedly on the minds of countless schoolchildren in late 1958. In the days leading up to the big reveal, more than 10,000 guesses were sent to Ta Hwa Publishing Co (大華文化社) for a chance to win prizes. The smash success of the comic series Great Battle Against the Demon Gang (大戰魔鬼黨) came as a surprise to author Yeh Hung-chia (葉宏甲), who had long given up on his dream after being jailed for 10 months in 1947 over political cartoons. Protagonist