For a parent, there is perhaps no greater fear than the prospect of losing a child to illness or accident, and it is childhood cancer that has the greatest potential to catapult a remote fear into an unimaginable reality. As a pediatric oncologist, having cared for children with cancer and their families for more than 25 years, I know that only a parent who has confronted such a diagnosis truly understands the depth of this fear, as it touches the core of who we are as parents.
I also know that we are treating more children more effectively than ever before — and that we can do better still.
For a child born in the 1960s, the diagnosis of the most common form of childhood cancer, acute lymphoblastic leukemia (ALL), meant almost certain death, with a survival rate of less than 10 percent. A child with the same diagnosis today has a better than 80 percent chance of being cured. Looking at the five-year survival rates for children with ALL from the 1970s through the 1990s, one sees an almost linear improvement in cure rates.
This makes the 1970s, 1980s and 1990s look like an era of accelerating discovery and therapeutic development. However, virtually all of the drugs that we use today to cure children with cancer were discovered and approved in the 1950s and 1960s. So, if new drugs did not fuel four decades of progress, what did?
A major driver was a remarkable, sustained scientific collaboration. In the 1950s, a group of clinical scientists recognized that, because childhood cancer was a rare disease, no single medical center could study enough patients to make the necessary advances across the spectrum of pediatric oncologic diseases. The decision to conduct collaborative research across multiple institutions resulted in the development of cooperative group research.
In the fight against childhood cancer, this concept evolved into what is now the Children’s Oncology Group, which unites more than 8,000 experts at more than 200 leading children’s hospitals, universities and cancer centers across the US, Australia, New Zealand and parts of Europe. The group conducts research across the spectrum of cancers that afflict children and has approximately 100 clinical trials underway around the world.
With an emerging infrastructure in place for cooperative research, sustained improvement in outcomes partly reflected an ever-increasing understanding that childhood cancers are diverse. Childhood ALL, for example, is not a single disease, but rather a spectrum of diseases. Recognition of this diversity led to the study of different treatment regimens in different sub-populations of children with pathologically similar cancers.
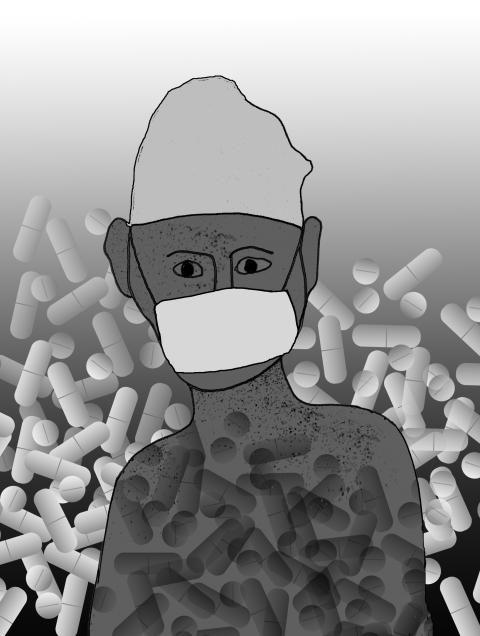
Throughout this period, the ability to overcome the most common side effect of cancer drugs, myelosuppression (a decrease in blood counts), improved dramatically. It began with the ability to transfuse not only red blood cells into anemic patients, but also platelets, reducing the threat of life-threatening bleeding that can accompany cancer therapy.
Equally important, the risks and types of life-threatening infections that come with myelosuppression were increasingly recognized, leading to the development and better use of more effective antibiotics. Starting in the 1990s, cytokines — drugs that stimulate bone marrow to produce infection-fighting white blood cells — began to be integrated into cancer treatments, further mitigating the risk of life-threatening infectious complications of care.
As a result of these advances in science and supportive care, the same chemotherapeutic drugs could be delivered much more intensively for children with select types and sub-types of cancer.
With selective intensification, cure rates began to increase steadily.
However, while this strategy has resulted in better outcomes, the acute and long-term morbidity of therapy has been substantial. Children with high-risk cancers who receive dose-intensive chemotherapy have a greater than 80 percent chance of experiencing at least one severe, life-threatening or fatal drug-related toxic event over the course of their treatment.
The late effects of cancer treatment include permanent organ and tissue damage, hormonal and reproductive dysfunction and second cancers.
More than 40 percent of the estimated 330,000 survivors of childhood cancer in the US experience a significant health-related complication from childhood cancer and its treatment. Despite our advances, cancer in developed countries remains the leading cause of death from disease in children older than one year.
We are, however, entering an era of unprecedented discovery. The powerful research tools that are now available to uncover the underlying basis of childhood cancers could fundamentally change how we treat children with these dreaded diseases. For a limited number of childhood cancers, there are new drugs that can target the fundamental drivers of malignancy. The most notable example is the impact of Gleevec (imatinib mesylate) on outcomes for children with an uncommon subtype of leukemia — Philadelphia chromosome-positive ALL.
The addition of this inhibitor to intensive chemotherapy has dramatically improved the outlook for these children, increasing the rate of three-year event-free survival from 35 percent to 80 percent. The development of targeted new agents is likely to affect outcomes for other subtypes of childhood cancer, including anaplastic large-cell lymphoma and other types of leukemias.
Given that childhood cancers are all rare or ultra-rare diseases, the ability of the biopharmaceutical industry to invest resources into development of new treatments is limited at best. Yet research is needed to identify potential targets for the entire spectrum of childhood cancers. For some potential targets, public-private partnerships will be needed to develop new therapeutic approaches.
The past 40 years have demonstrated the remarkable return on investment to be gained in collaborative scientific research. Now we must leverage current scientific opportunities and invest the resources needed to develop more effective, less toxic therapies, thereby improving outcomes for all children with cancer.
Peter Adamson is chair of the Children’s Oncology Group at the Children’s Hospital of Philadelphia.
Copyright: Project Syndicate

Because much of what former US president Donald Trump says is unhinged and histrionic, it is tempting to dismiss all of it as bunk. Yet the potential future president has a populist knack for sounding alarums that resonate with the zeitgeist — for example, with growing anxiety about World War III and nuclear Armageddon. “We’re a failing nation,” Trump ranted during his US presidential debate against US Vice President Kamala Harris in one particularly meandering answer (the one that also recycled urban myths about immigrants eating cats). “And what, what’s going on here, you’re going to end up in World War
Earlier this month in Newsweek, President William Lai (賴清德) challenged the People’s Republic of China (PRC) to retake the territories lost to Russia in the 19th century rather than invade Taiwan. He stated: “If it is for the sake of territorial integrity, why doesn’t [the PRC] take back the lands occupied by Russia that were signed over in the treaty of Aigun?” This was a brilliant political move to finally state openly what many Chinese in both China and Taiwan have long been thinking about the lost territories in the Russian far east: The Russian far east should be “theirs.” Granted, Lai issued
On Tuesday, President William Lai (賴清德) met with a delegation from the Hoover Institution, a think tank based at Stanford University in California, to discuss strengthening US-Taiwan relations and enhancing peace and stability in the region. The delegation was led by James Ellis Jr, co-chair of the institution’s Taiwan in the Indo-Pacific Region project and former commander of the US Strategic Command. It also included former Australian minister for foreign affairs Marise Payne, influential US academics and other former policymakers. Think tank diplomacy is an important component of Taiwan’s efforts to maintain high-level dialogue with other nations with which it does

On Sept. 2, Elbridge Colby, former deputy assistant secretary of defense for strategy and force development, wrote an article for the Wall Street Journal called “The US and Taiwan Must Change Course” that defends his position that the US and Taiwan are not doing enough to deter the People’s Republic of China (PRC) from taking Taiwan. Colby is correct, of course: the US and Taiwan need to do a lot more or the PRC will invade Taiwan like Russia did against Ukraine. The US and Taiwan have failed to prepare properly to deter war. The blame must fall on politicians and policymakers