The first fatal case of dengue fever this year has been reported in Pingtung and was among the 13 locally acquired dengue infections confirmed last week, the Centers for Disease Control (CDC) said yesterday.
Five imported and 13 locally acquired cases of dengue infection were reported last week, with all of the locally acquired cases coming from Pingtung County, the centers said, adding that 152 of the total 164 locally acquired infections confirmed so far this year were reported in the county, with the remainder reported in Taipei, New Taipei City (新北市) and Greater Kaohsiung.
The fatal case involved a 76-year-old woman with a history of high blood pressure who started to exhibit symptoms of loss of appetite, dry mouth, headache, nausea, vomiting, diarrhea, muscle pain and joint pain on Oct. 6 and was diagnosed with dengue infection after seeking medical attention.
She fell unconscious after falling down several times on Thursday, and died the next day, despite being taken to an emergency room for treatment, the centers said.
“She was diagnosed with intracerebral hemorrhage when she was taken to the hospital after her falls. So the direct cause of death was a brain hemorrhage as a result of her falls,” CDC physician Philip Lo Yi-chun (羅一鈞) said.
“Her death was associated with dengue fever because the infection had caused [a low platelet count in her blood]. The dengue infection and the decrease of platelets in her blood were the indirect cause of her death,” he said.
Three of the woman’s four family members have since been diagnosed with dengue fever, the centers added.
The centers reiterated the importance of domestic hygiene and the need to eliminate potential mosquito breeding sites to reduce mosquito density in surrounding communities.
Meanwhile, the centers said 117 cases of acute hepatitis A virus (HAV) have been reported this year as of Saturday last week, underscoring the importance of food hygiene as 40 percent of the cases had reported a history of eating raw food.
Eighty-six of the 117 reported acute HAV infections were locally acquired and 31 were imported, the centers said.
Further investigations have showed that 40 percent of the infected had eaten raw food at some point before the onset of the disease, of which 36 percent reported to have eaten raw seafood.
High-risk food items associated with HAV infection include shellfish, such as raw oysters, mollusks and scallops, fruits, such as frozen blueberries and raspberries and semi-dried tomatoes, and raw scallions and salads.
As sanitary conditions have improved in the past years, most children and teenagers do not have antibodies against the virus, and are susceptible to infection when coming into contact with virus-contaminated food and water, the centers said.
Following good food hygiene practices, the Food and Drug Administration has listed HAV screening as one of the mandatory tests to be done at food handlers’ health examinations to reduce the risk of the virus spreading through food.
HAV is passed on via the fecal-oral route by consuming HAV-contaminated food or water, the centers said.
The incubation period for the disease ranges between 15 days and 50 days, with those infected experiencing symptoms such as fever, fatigue, loss of appetite, vomiting and abdominal pain, before developing jaundice a few days later.
The centers said that most people recover from HAV without medical help and develop a lifelong immunity to the disease.
While the mortality rate is relatively low at about one per thousand, elderly people and those with chronic hepatitis B or C or underlying liver disease are at higher risk of acute sudden hepatic failure.
The centers reminded those without anti-HAV antibodies to receive two doses of hepatitis A vaccine and to avoid eating raw or undercooked food.
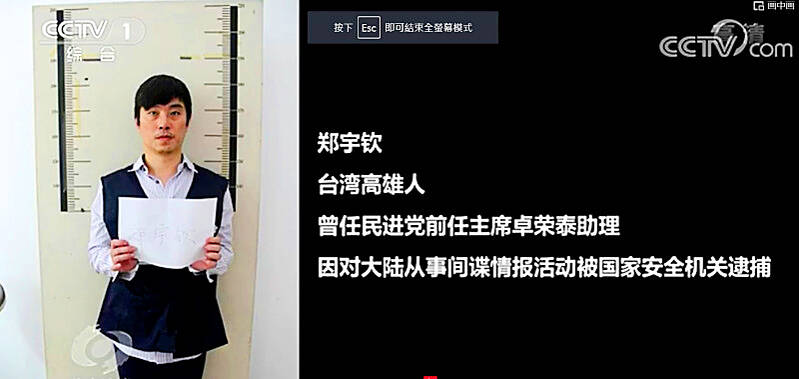
Former Czech Republic-based Taiwanese researcher Cheng Yu-chin (鄭宇欽) has been sentenced to seven years in prison on espionage-related charges, China’s Ministry of State Security announced yesterday. China said Cheng was a spy for Taiwan who “masqueraded as a professor” and that he was previously an assistant to former Cabinet secretary-general Cho Jung-tai (卓榮泰). President-elect William Lai (賴清德) on Wednesday last week announced Cho would be his premier when Lai is inaugurated next month. Today is China’s “National Security Education Day.” The Chinese ministry yesterday released a video online showing arrests over the past 10 years of people alleged to be

THE HAWAII FACTOR: While a 1965 opinion said an attack on Hawaii would not trigger Article 5, the text of the treaty suggests the state is covered, the report says NATO could be drawn into a conflict in the Taiwan Strait if Chinese forces attacked the US mainland or Hawaii, a NATO Defense College report published on Monday says. The report, written by James Lee, an assistant research fellow at Academia Sinica’s Institute of European and American Studies, states that under certain conditions a Taiwan contingency could trigger Article 5 of NATO, under which an attack against any member of the alliance is considered an attack against all members, necessitating a response. Article 6 of the North Atlantic Treaty specifies that an armed attack in the territory of any member in Europe,

LIKE FAMILY: People now treat dogs and cats as family members. They receive the same medical treatments and tests as humans do, a veterinary association official said The number of pet dogs and cats in Taiwan has officially outnumbered the number of human newborns last year, data from the Ministry of Agriculture’s pet registration information system showed. As of last year, Taiwan had 94,544 registered pet dogs and 137,652 pet cats, the data showed. By contrast, 135,571 babies were born last year. Demand for medical care for pet animals has also risen. As of Feb. 29, there were 5,773 veterinarians in Taiwan, 3,993 of whom were for pet animals, statistics from the Animal and Plant Health Inspection Agency showed. In 2022, the nation had 3,077 pediatricians. As of last

XINJIANG: Officials are conducting a report into amending an existing law or to enact a special law to prohibit goods using forced labor Taiwan is mulling an amendment prohibiting the importation of goods using forced labor, similar to the Uyghur Forced Labor Prevention Act (UFLPA) passed by the US Congress in 2021 that imposed limits on goods produced using forced labor in China’s Xinjiang region. A government official who wished to remain anonymous said yesterday that as the US customs law explicitly prohibits the importation of goods made using forced labor, in 2021 it passed the specialized UFLPA to limit the importation of cotton and other goods from China’s Xinjiang Uyghur region. Taiwan does not have the legal basis to prohibit the importation of goods