Led by Mackay Memorial Hospital’s Department for Pediatric Hematology-Oncology, Taiwan has used intrathecal chemotherapy as the treatment of choice for childhood acute lymphoblastic leukemia (ALL) since 2009, and the treatment can decrease the rate of central nervous system relapses and avoid the long-term pathological conditions caused by prophylactic cranial irradiation, the hospital said yesterday.
ALL is the most common cancer among children, affecting one in every four children who have cancer.
Traditionally, the disease had been treated by administering cranial irradiation and intrathecal chemotherapy injections, department director Liu His-che (劉希哲) said.
However, the Mackay Memorial Hospital dropped the use of prophylactic irradiation in 1999 to avoid the serious complications and chronic conditions that it could cause, such as brain tumors, neurocognitive deficits, endocrinopathy — a hormone imblance — and short stature.
Liang Der-cherng (梁德成), an attending physician at the department, who has headed the establishment of a national treatment protocol for childhood ALL since 1993, said that the lumbar puncture required by intrathecal chemotherapy, which was usually done at the time of diagnosis, has also been delayed in the new procedure.
Performing the lumbar puncture before circulating cancer cells are first eliminated by chemotherapeutic drugs can result in cancer cells in the blood being taken to the brain, Liang said, adding that this could inadvertently complicate the disease.
“Mackay has treated 152 children with ALL since 1999 with treatment that omitted prophylactic cranial irradiation and nearly 90 percent of them were cured, with no cases of isolated central nervous system relapses and a combined central nervous system relapse rate of just 1.4 percent,” Liu said.
Another strategy that has furthered the success of treating ALL is measuring the level of minimal residual leukaemic cells to accurately predict the risk of relapse, and determine and adjust the intensity of therapy, Liu said.
“It’s better to have a minimal residual leukemia level lower than 0.01 percent, which is one leukemic cell among 10,000 normal cells,” Liu said.
The hospital said that in January, the measurement was integrated into the latest national treatment procedure for ALL.
However, the measurement is not covered by National Health Insurance.
Each patient needs multiple minimal residual leukemia measurements, and each test costs more than NT$20,000, which can be a huge financial burden especially for low-income families, said the two doctors, who also called on the society to support the new treatment by way of donations.

A group of Taiwanese-American and Tibetan-American students at Harvard University on Saturday disrupted Chinese Ambassador to the US Xie Feng’s (謝鋒) speech at the school, accusing him of being responsible for numerous human rights violations. Four students — two Taiwanese Americans and two from Tibet — held up banners inside a conference hall where Xie was delivering a speech at the opening ceremony of the Harvard Kennedy School China Conference 2024. In a video clip provided by the Coalition of Students Resisting the CCP (Chinese Communist Party), Taiwanese-American Cosette Wu (吳亭樺) and Tibetan-American Tsering Yangchen are seen holding banners that together read:

UNAWARE: Many people sit for long hours every day and eat unhealthy foods, putting them at greater risk of developing one of the ‘three highs,’ an expert said More than 30 percent of adults aged 40 or older who underwent a government-funded health exam were unaware they had at least one of the “three highs” — high blood pressure, high blood lipids or high blood sugar, the Health Promotion Administration (HPA) said yesterday. Among adults aged 40 or older who said they did not have any of the “three highs” before taking the health exam, more than 30 percent were found to have at least one of them, Adult Preventive Health Examination Service data from 2022 showed. People with long-term medical conditions such as hypertension or diabetes usually do not
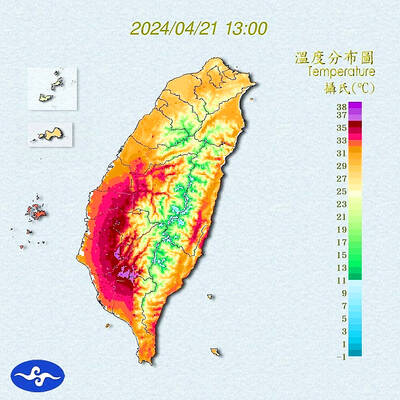
Heat advisories were in effect for nine administrative regions yesterday afternoon as warm southwesterly winds pushed temperatures above 38°C in parts of southern Taiwan, the Central Weather Administration (CWA) said. As of 3:30pm yesterday, Tainan’s Yujing District (玉井) had recorded the day’s highest temperature of 39.7°C, though the measurement will not be included in Taiwan’s official heat records since Yujing is an automatic rather than manually operated weather station, the CWA said. Highs recorded in other areas were 38.7°C in Kaohsiung’s Neimen District (內門), 38.2°C in Chiayi City and 38.1°C in Pingtung’s Sandimen Township (三地門), CWA data showed. The spell of scorching

POLICE INVESTIGATING: A man said he quit his job as a nurse at Taipei Tzu Chi Hospital as he had been ‘disgusted’ by the behavior of his colleagues A man yesterday morning wrote online that he had witnessed nurses taking photographs and touching anesthetized patients inappropriately in Taipei Tzu Chi Hospital’s operating theaters. The man surnamed Huang (黃) wrote on the Professional Technology Temple bulletin board that during his six-month stint as a nurse at the hospital, he had seen nurses taking pictures of patients, including of their private parts, after they were anesthetized. Some nurses had also touched patients inappropriately and children were among those photographed, he said. Huang said this “disgusted” him “so much” that “he felt the need to reveal these unethical acts in the operating theater