Ira’s story is a classic example of invasive cardiology run amok. Ira, of Hewlett, New York, was 53 when he had an exercise stress test as part of an insurance policy application. Though he lasted the full 12 minutes on the treadmill with no chest pain, an abnormality on the EKG led to an angiogram, which prompted the cardiologist to suggest that a coronary artery narrowed by atherosclerosis be widened by balloon angioplasty, with a wire-mesh tube called a stent inserted to keep the artery open.
The goal, he was told, was to prevent a clot from blocking the artery and causing a heart attack or sudden cardiac death.
Wanting to avoid an invasive procedure, Ira decided to pursue a less drastic course of dieting, weight loss and cholesterol-lowering medication. But three years later, the specter of a stent arose again. An abnormal reading on a pre-surgical EKG led to another angiogram, which indicated that the original narrowing had worsened. Cowed by the stature of the cardiologist, Ira finally agreed to have not one but three coronary arteries treated with angioplasty and drug-coated stents, making him one of about a million Americans who last year underwent angioplasties, most of whom had stents inserted.
For patients in the throes of a heart attack and those with crippling chest pain from even minor exertion, angioplasty and stents can be lifesaving, says Michael Ozner, a Miami cardiologist and the author of The Great American Heart Hoax. But, Ozner said in an interview, such “unstable” patients represent only a minority of those undergoing these costly and sometimes risky procedures.
Most stent patients are healthy like Ira, who was experiencing no chest pain or cardiac symptoms of any sort. Yet Ira was afraid not to follow the doctor’s advice, despite the fact that no study has shown that these procedures in otherwise healthy patients can reduce the risk of heart attacks, crippling angina or sudden cardiac death. “We’ve extended the indications for surgical angioplasty and stent placement without any data to support the procedures in the vast majority of patients — stable patients with blockages in their arteries,” Ozner said.
What the studies do show, Ozner said, is that putting stents in such patients is no more protective than following a heart-healthy lifestyle and taking medication and, if necessary, nutritional supplements to reduce cardiac risk. The studies have also shown that stents sometimes make matters worse by increasing the chance that a dangerous clot will form in a coronary artery, as noted in 2006 by an advisory panel to the US Food and Drug Administration.
Ozner, medical director of the Cardiovascular Prevention Institute of South Florida, is one of many prevention-oriented cardiologists vocal about the overuse of “interventional cardiology,” a specialty involving invasive coronary treatments that have become lucrative for the hospitals and doctors who perform them.
Even some interventional cardiologists have expressed concern about the many patients without symptoms who are treated surgically. “The only justification for these procedures is to prolong life or improve the quality of life,” said David Brown, an interventional cardiologist and chief of cardiology at Stony Brook University Medical Center, “and there are plenty of patients undergoing them who fit into neither category.”
The treatments — coronary artery bypass surgery, angioplasty and the placement of drug-coated stents — cost about US$60 billion a year in the US. Though they are not known to prevent heart attacks or coronary mortality in most patients, they are covered by insurance. Counseling patients about diet, exercise and stress management — which is relatively inexpensive and has been proved to be life-extending — is rarely reimbursed. In other words, procedure-oriented modern cardiology is pound wise and penny foolish. And in these economic times, it makes great sense to reconsider the approaches to reducing morbidity and mortality from the nation’s leading killer.
Most people mistakenly think of coronary artery disease as a plumbing problem. Influenced by genetics, diet, diabetes, hypertension, smoking and other factors, major arteries through which oxygen-rich blood flows to the heart gradually become narrowed by deposits of cholesterol-rich plaques until blood can no longer pass through, resulting in a heart attack.
In coronary bypass surgery, a blood vessel taken from elsewhere in the body is reattached to a clogged coronary artery to bypass the narrowed part.
However, as Ozner points out in his book, “three major studies performed in the late 1970s and early 1980s clearly proved that for the majority of patients, bypass surgery is no more effective than conservative medical treatment.” The exceptions — patients whose health and lives could be saved — were those with advanced disease of the left main coronary artery and those with severe crippling, or unstable, angina.
Bypass surgery does relieve the pain of angina, though recent studies suggest this may happen because pain receptors around the heart are destroyed during surgery.
“The studies on angioplasty delivered even worse news,” Ozner wrote. “Unless the patient was in the midst of a heart attack, the opening of a blocked coronary artery with a balloon catheter resulted in a worse outcome compared to management through medication.” In fact, one trial, published in 2003 in the Journal of the American College of Cardiology, found that balloon angioplasty, which flattens plaque against arterial walls, actually raised the risk of a heart attack or death.
Stents were designed to keep the flattened plaque in place. But studies of stable patients found no greater protection against heart attacks from stents than from treatments like making lifestyle changes and taking drugs to lower cholesterol and blood pressure.
A new understanding of how most heart attacks occur suggests why these procedures have not lived up to their promise. According to current evidence, most heart attacks do not occur because an artery is closed by a large plaque. Rather, a relatively small, unstable plaque ruptures and attracts inflammatory cells and coagulating agents, leading to an artery-blocking clot.
In most Americans middle aged and older, small plaques are ubiquitous in coronary arteries and there is no surgical way to treat them all.
“Interventional cardiology is doing cosmetic surgery on the coronary arteries, making them look pretty, but it’s not treating the underlying biology of these arteries,” said Ozner, who received the 2008 American Heart Association Humanitarian Award. “If some of the billions spent on intervention were put into prevention, we’d have a much healthier America at a lower cost.”
Ozner advises patients who are told they need surgery to get an independent second opinion from a specialist.

In late October of 1873 the government of Japan decided against sending a military expedition to Korea to force that nation to open trade relations. Across the government supporters of the expedition resigned immediately. The spectacle of revolt by disaffected samurai began to loom over Japanese politics. In January of 1874 disaffected samurai attacked a senior minister in Tokyo. A month later, a group of pro-Korea expedition and anti-foreign elements from Saga prefecture in Kyushu revolted, driven in part by high food prices stemming from poor harvests. Their leader, according to Edward Drea’s classic Japan’s Imperial Army, was a samurai

The following three paragraphs are just some of what the local Chinese-language press is reporting on breathlessly and following every twist and turn with the eagerness of a soap opera fan. For many English-language readers, it probably comes across as incomprehensibly opaque, so bear with me briefly dear reader: To the surprise of many, former pop singer and Democratic Progressive Party (DPP) ex-lawmaker Yu Tien (余天) of the Taiwan Normal Country Promotion Association (TNCPA) at the last minute dropped out of the running for committee chair of the DPP’s New Taipei City chapter, paving the way for DPP legislator Su
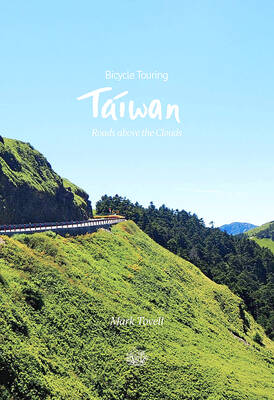
It’s hard to know where to begin with Mark Tovell’s Taiwan: Roads Above the Clouds. Having published a travelogue myself, as well as having contributed to several guidebooks, at first glance Tovell’s book appears to inhabit a middle ground — the kind of hard-to-sell nowheresville publishers detest. Leaf through the pages and you’ll find them suffuse with the purple prose best associated with travel literature: “When the sun is low on a warm, clear morning, and with the heat already rising, we stand at the riverside bike path leading south from Sanxia’s old cobble streets.” Hardly the stuff of your

Located down a sideroad in old Wanhua District (萬華區), Waley Art (水谷藝術) has an established reputation for curating some of the more provocative indie art exhibitions in Taipei. And this month is no exception. Beyond the innocuous facade of a shophouse, the full three stories of the gallery space (including the basement) have been taken over by photographs, installation videos and abstract images courtesy of two creatives who hail from the opposite ends of the earth, Taiwan’s Hsu Yi-ting (許懿婷) and Germany’s Benjamin Janzen. “In 2019, I had an art residency in Europe,” Hsu says. “I met Benjamin in the lobby